Autologous Stromal Vascular Fraction Therapy for Rheumatoid Arthritis: Rationale and Clinical Safety
Paz Rodriguez J, Murphy M, Hong S, Madrigal M, March K, Minev B, Harman R, Chen CS, Berrocal Timmons R, Marleau A, Riordan N – International Archives of Medicine 2012, 5:5
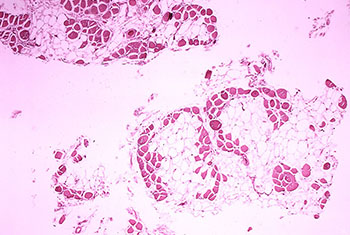
Advancements in rheumatoid arthritis (RA) treatment protocols and introduction of targeted biological therapies have markedly improved patient outcomes, despite this, up to 50% of patients still fail to achieve a significant clinical response. In veterinary medicine, stem cell therapy in the form of autologous stromal vascular fraction (SVF) is an accepted therapeutic modality for degenerative conditions with 80% improvement and no serious treatment associated adverse events reported. Clinical translation of SVF therapy relies on confirmation of veterinary findings in targeted patient populations. Here we describe the rationale and preclinical data supporting the use of autologous SVF in treatment of RA, as well as provide 1, 3, 6, and 13 month safety outcomes in 13 RA patients treated with this approach.
Syndrome, Lipodystrophy, and Aging Be Mesenchymal Stem Cell Exhaustion Syndromes?
Eduardo Mansilla,* Vanina Díaz Aquino, Daniel Zambón, Gustavo Horacio Marin, Karina Mártire, Gustavo Roque, Thomas Ichim, Neil H. Riordan, Amit Patel, Flavio Sturla, Gustavo Larsen, Rubén Spretz, Luis Núñez, Carlos Soratti, Ricardo Ibar, Michiel van Leeuwen, José María Tau, Hugo Drago, and Alberto Maceira – Stem Cells Int. 2011; 2011: 943216
One of the most important and complex diseases of modern society is metabolic syndrome. This syndrome has not been completely understood, and therefore an effective treatment is not available yet. We propose a possible stem cell mechanism involved in the development of metabolic syndrome. This way of thinking lets us consider also other significant pathologies that could have similar etiopathogenic pathways, like lipodystrophic syndromes, progeria, and aging. All these clinical situations could be the consequence of a progressive and persistent stem cell exhaustion syndrome (SCES). The main outcome of this SCES would be an irreversible loss of the effective regenerative mesenchymal stem cells (MSCs) pools. In this way, the normal repairing capacities of the organism could become inefficient. Our point of view could open the possibility for a new strategy of treatment in metabolic syndrome, lipodystrophic syndromes, progeria, and even aging: stem cell therapies.

Feasibility of combination allogeneic stem cell therapy for spinal cord injury: a case report
Thomas E. Ichim, Fabio Solano, Fabian Lara, Eugenia Paris, Federico Ugalde, Jorge Paz Rodriguez,
Boris Minev, Vladimir Bogin, Famela Ramos, Erik J Woods, Michael P Murphy, Amit N Patel,
Robert J Harman, Neil H. Riordan – International Archives of Medicine 2010, 3:30
Cellular therapy for spinal cord injury (SCI) is overviewed focusing on bone marrow mononuclear cells, olfactory ensheathing cells, and mesenchymal stem cells. A case is made for the possibility of combining cell types, as well as for allogeneic use.